GBMC Health Partners Orthopaedics
A multidisciplinary approach to patient care aimed at maximizing recovery efforts and restoring quality of life
A full range of orthopaedic services are available, including: non-surgical outpatient treatments, consultations and physical therapy, fracture repair, minimally invasive total and partial joint replacements, and complex spine procedures. Patient education is an integral component to the patient experience, with pre-operative education and planning classes for both patients and family members.
GBMC’s orthopaedic surgeons continually lead their fields in new clinical technologies, and patients benefit from clinical trial participation. New, minimally invasive arthroscopic techniques allow surgeons to perform many procedures on an outpatient basis including, but not limited to, arthroscopy, total joint replacement, partial knee replacement, foot and ankle reconstruction, arthritis and fracture care.
- Achilles Repair
- ACL Reconstruction
- Adult Reconstruction Hip & Knee
- Ankle Arthroscopy
- Bunionectomy
- Carpal Tunnel Surgery
- Direct Anterior & Mini Posterior Hip Replacement
- Flatfoot Correction
- Foot/Ankle Fractures and Fusions
- Fracture Fixation
- Fracture Repair
- Hammer Toe and Claw Toe Correction
- Hip Replacement
- Knee & Shoulder Surgery
- Knee Arthroscopy
- Knee Replacement
- Minimally Invasive Techniques
- Partial and Total Knee Replacement
- Rapid Recovery Program
- Rotator Cuff Repair
- Shoulder Arthroscopy
- Shoulder Stabilization
- Total Ankle Replacement
- Total Joint Replacment
- Total Shoulder Replacement
- Ultrasound Guided Arthrocentesis
- Achilles Tendon Rupture
- Ankle Arthritis
- Ankle Fractures
- Ankle Sprains (High Ankle Sprain)
- Arthritic Knees and Hips
- Arthritis Injuries
- Avascular Necrosis
- Bunions/Hallux Valgus
- Bursitis Tendonitis
- Carpal Tunnel
- Degenerative Joint Disease
- ED Trauma
- Fractures
- General Orthopaedics
- Hammertoes
- Hip Fractures
- Knee and Shoulder Arthritis
- Knee Injury
- Ligament Tears (MCL, ACL)
- Meniscus Tears
- Osteoarthritis
- Osteopenia
- Osteoporosis
- Patella Tendonitis
- Pelvic Fractures
- Plantar Fasciitis
- Recurrent fractures
- Rotator Cuff Tears
- Shoulder Dislocations
- Sports Injuries
- Tendon Tears
- Tendonitis
- Trigger Finger
Orthopaedics Walk-in Clinic
The Orthopaedic Walk-in Clinic is now available at two locations - GBMC Main Campus and Padonia Road!
GBMC Main Campus
6569 N. Charles Street, Physicians Pavilion West, Suite 705
Monday–Friday, 8 a.m. - 3 p.m. (last patient at 2:30 p.m.)
GBMC Health Partners Primary Care Padonia
63 E. Padonia Rd., Suite 100, Timonium MD 21093
Monday - Friday, 8 a.m. - 3 p.m. (last patient at 2:30 p.m.)
Saturday, 8 a.m. - 12 p.m. (last patient at 11:30 a.m.)
*Note
-
Hours are subject to change. Please contact the office at 443-849-3838 for additional details.
-
An insurance referral may be required upon arrival. Please check your insurance coverage prior to your visit to determine whether you need a referral.
Our Services
We offer a wide variety of surgical interventions for a number of different conditions including:
- Foot & Ankle Conditions
- Hip Conditions
- Knee Conditions
- Physical Medicine and Rehabilitation
- Shoulder & Elbow Conditions
- Sports Medicine
- Total Joint Replacement
- Osteoporosis Care
- Bone Optimization prior to Surgery
- Fracture Prevention

Total Knee Replacement Gets Patient Back in Motion
“We first tried a conservative approach of cortisone shots and physical therapy to strengthen the muscles surrounding my knee,” Mrs. Speca explains. When the pain persisted despite the treatment, she and Dr. Schmidt discussed and agreed upon the surgical option of a total knee replacement.
Hip Replacement
The healthy hip is a ball-and-socket joint. The ball is at the top of the thighbone (femur), and the socket (acetabulum) is in the hipbone (pelvis). The connection allows the leg to move in a variety of positions. The ball and socket are each covered with cartilage that lubricates and cushions the bones during movement.
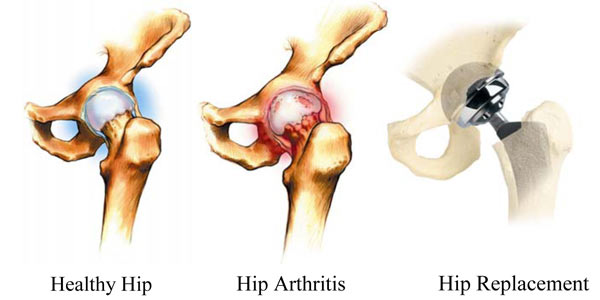
Arthritis is a term that is used to describe over 100 different kinds of conditions that can affect the human body. There are millions of Americans who are affected by arthritis each year. Arthritis can cause pain, stiffness, swelling, and loss of motion in affected joints.
The bones in the hip are exposed by an incision. The damaged sections of bone are removed to make room for the replacement components. The thighbone receives a metal alloy stem and ball, and the pelvis receives a metal cup and liner. Traditionally, the metal cup is lined with polyethylene (plastic) to act as healthy cartilage. However, modern technology has allowed advancements in both metal and ceramic liners. These components now give the patient and surgeon additional options for hip replacement. Your surgeon will evaluate your specific condition and may be able to tell you which option will provide the most favorable results.
|

|

|

|
During your first few weeks at home, it is important that you move properly. You should avoid crossing your legs while sitting or standing, and do not allow your knees to come higher than your hips. Also, avoid sitting in low sofas or chairs.
It is important to have some assistance when going up and down stairs. When climbing stairs, always use the railing and lead with your non-surgical leg, one step at a time. When going down stairs, hold onto the railing and lead with your surgical leg, again, one step at a time.
Continue the prescribed exercises during your entire recovery period, and talk to your doctor about developing an exercise program after you fully recover. Golfing, swimming, walking, and bicycling are excellent sources of low-impact exercise if your physician feels that these activities are appropriate for your individual condition.
Follow your physician's check-up plan. It is common to visit with your surgeon at three, six, and nine months after surgery and annually thereafter.
Knee Replacement
The healthy knee is a hinge joint. The three bones that form the knee are the thighbone (femur), shinbone (tibia), and kneecap (patella). The femur and tibia are held together by ligaments, which are strong bands of tissue that stabilize the joint. The end of the femur, the top of the tibia, and the back of the patella are covered with a tough lubricating tissue called cartilage. Cartilage acts like a natural shock absorber, preventing both bone on bone contact and providing a smooth, pain-free surface for the bones to glide against. The knee also contains synovial membranes, which produce synovial fluid to help lubricate and nourish the cartilage.
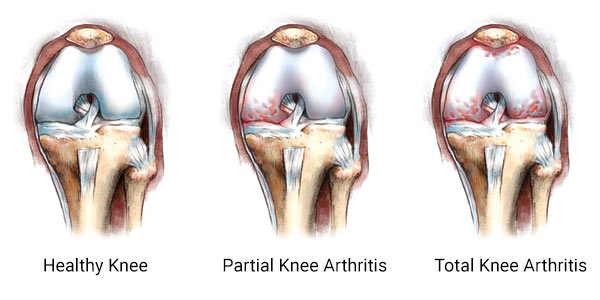
Knee cartilage can be compared to the tread of an automobile tire, very durable but susceptible to wear over time. Osteoarthritis is a degenerative process, which results in the wearing out of the cartilage that protects the bones in the joints. As we age, the tread surface slowly erodes until the underlying bone is exposed. This exposed bone can be painful when the joint moves and bears weight.
Arthritis is a term that is used to describe over 100 different kinds of conditions that can affect the human body. Arthritis affects millions of Americans each year with symptoms including pain, stiffness, swelling, and loss of motion in affected joints.
Total knee replacement, also called total knee arthroplasty, uses metal alloy and polyethylene (plastic) components to resurface the bones in the joint. The implants are designed to re-create the shape of the bones in a healthy joint.
The end of the thighbone can be compared to a rocking chair. It has two distinct surfaces, or rockers, that contact the top of the shinbone. Each rocker is called a condyle, and there are two condyles at the end of the thighbone. The femoral component re-creates each rocker at the end of the thighbone. The top of the tibia is covered with a metal tray that is used to support the polyethylene plastic bearing. The polyethylene acts as the joint's natural cartilage, absorbing stress and providing smooth movement. The polyethylene on the back of the kneecap also provides smooth movement against the femoral component.

|

|

|

|
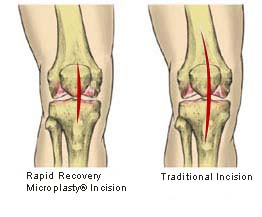
The field of orthopedics is constantly researching new techniques to help make joint replacement surgery less painful and to help patients recover more quickly. One of the most talked about orthopedic advancements is Microplasty® minimally invasive joint replacement, also called mini-incision joint replacement. Traditional total knee replacements require an incision between eight and ten inches long. The patient's size and the extent of the joint's damage can sometimes determine the length of the incision. The incision allows the surgeon to fully visualize the joint, the diseased tissue, and the implants. Rapid Recovery Microplasty® minimally invasive total knee replacement may be performed through a four to six inch incision, half the length of a typical knee replacement incision. Surgeons can perform surgery through such a short incision because they use instruments specifically designed to move around soft tissue, rather than cut through it.
It is important to remember that surgeons still use the clinically proven implants that they feel will best treat your specific condition.
Why are Surgeons Performing Rapid Recovery Minimally Invasive Knee Replacement?
Today's implants offer exceptional outcomes, but traditional surgical techniques require a long and involved physical recovery. Surgeons understand that patients desire to heal quickly so they can return to a more active and enjoyable lifestyle.
In addition to a shorter incision, surgeons using the Rapid Recovery Program have implemented a highly organized treatment plan for their patients' physical and mental health. Rapid Recovery patients are educated with a variety of materials. The comprehensive educational materials will help patients understand the surgical procedure and its outcomes.
Rapid Recovery patients begin preoperative strengthening exercises to help them prepare for surgery and their recovery. Patients may be given a comprehensive nutrition plan to help ensure optimum health before surgery.
Rapid Recovery surgeons may also implement a unique pain program during surgery that is designed to dramatically reduce a patient's postoperative pain. Reducing patients' postoperative pain is critical to helping them begin their postoperative rehabilitation and to helping them make a Rapid Recovery.
Complications
While uncommon, complications can occur during and after surgery. Some complications include infection, blood clots, implant breakage, misalignment, and premature wear. Although implant surgery is extremely successful in most cases, some patients still experience stiffness and pain. No implant will last forever and factors such as the patient's post-surgical activities and weight can affect longevity. Be sure to discuss these and other risks with your surgeon.
There are many things that your surgeon may do to minimize the potential for complications. Your surgeon may have you see a medical physician before surgery to obtain tests. You may also need to have your dental work up to date and may be shown how to prepare your home to avoid falls.
After Surgery
After surgery, you probably will be hospitalized for two to three days. During this time, you will receive pain medication and begin physical therapy. It is important to start moving your new knee as soon as possible after surgery to promote blood flow, to regain knee motion, and to facilitate the Rapid Recovery process. You should be out of bed and walking with crutches or a walker within 24 hours of your surgery.
You will be shown how to safely climb and descend stairs, how to get into and out of a seated position, and how to care for your knee once you return home. It is a good idea to enlist the help of friends or family to help you once you do return home.
Before you leave the hospital, your therapist will show you a variety of exercises designed to help you regain mobility and strength in your knee. You should be able to perform these exercises on your own at home. When at home, it is important to continue with your exercises as your physician has instructed.
Rapid Recovery
Rapid Recovery after minimally invasive knee replacement takes approximately half as long as traditional total knee replacement. Every person's recovery time will vary, but most people should be able to drive after two weeks, garden after three to four weeks, and golf about six to eight weeks after surgery. Your surgeon will tell you when you can return to these activities and will also tell you which activities to avoid.
You will typically not be allowed to participate in high-impact activities or contact sports. These types of activities place extreme pressure on the joints, which could lead to complications.
Summary
We know the decision to have surgery is sometimes difficult. We hope this information has helped you understand some of the basics of Rapid Recovery Microplasty® minimally invasive knee replacement surgery so that you can make the best decision for yourself. Millions of others have made this choice, allowing them to return to more active lifestyles. This is not intended to replace the experience and counsel of your orthopedic surgeon. If you have any further questions, please speak with your orthopedic surgeon.