Self-Administered HPV Tests May Help to Increase Access, But Are Only Part of the Solution
January 16, 2026
In December 2025, the Food and Drug Administration (FDA) approved three self-administered tests to screen for human papillomavirus (HPV). Because 99% of cervical cancers are caused by HPV, the American Cancer Society updated its guidelines to include these tests as an approved method for cervical cancer screening. These approvals are promising and can provide greater accessibility for women.
Self-administered tests test specifically for HPV and should not replace gynecologic exams, which are still important for overall pelvic health. However, they may help to provide increased access and comfort for cervical cancer screening.
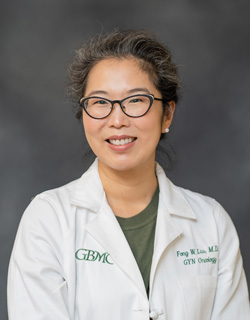
“Many patients may be interacting with the healthcare system for other reasons but not be seeing a gynecologist regularly and may be missing screening because of that,” Kimberly Levinson, MD, MPH, Director of Johns Hopkins Gynecologic Oncology at GBMC, said.
Most women are familiar with the term “Pap smear,” but is only part of what a gynecologist does during routine exams. Often, when women are swabbed, gynecologists collect specimens for cytology, which is an exam of the cells, as well as for HPV testing.
“There’s a period of life—often from the late 20s through the early 40s—when women may not be presenting to healthcare for themselves. They’re busy, they feel healthy, they’re caring for kids and/or parents. That’s one example of when screening can get missed,” Dr. Levinson said.
While research is ongoing, at this point, self-administered tests still need to be performed during a medical visit (either at a gynecology office, primary care office, or clinic setting) and processed through a medical lab. They may be useful for those who cannot tolerate speculum exams, or those who frequently interact with the healthcare system for other reasons, and adding another appointment for gynecologic care is an additional burden. While self-administered tests are currently recommended for average-risk individuals, they could, in the future, be helpful for patients at increased risk and require more frequent screening (for example: immunocompromised patients).
HPV can remain dormant for decades and cause cancer without early warning signs. Screening is often the only way to detect cervical precancers.
Most people who are not vaccinated will have HPV at some point in their lives and will clear it on their own. However, if HPV stays present in the cells of the cervix, it can then cause changes to those cervical cells leading to dysplasia or pre-cancer cells.
Positive HPV tests can put patients in a cycle of monitoring that includes screening, colposcopy, and biopsy every six months, which can be a painful and time-consuming process, but is the only way to properly monitor changes or developing cancer.
At GBMC, patients who receive abnormal HPV screening results are supported by a gynecologic oncology team that provides expert evaluation, follow-up testing, and individualized care plans. GBMC’s specialists focus on helping patients understand their results, navigate next steps, and feel supported throughout the process.
If cancer does develop, GBMC offers a full array of minimally invasive treatments that can preserve fertility. GBMC also provides patients access to national clinical trials that expand treatment options.
While self-administered tests provide an incredible opportunity to catch missing diagnoses, most practices are not yet set up to offer this service. Vaccination is still the recommended, most effective preventive measure. HPV vaccines are covered by insurance for patients 45 and younger and can protect against the most common high-risk HPV types.
“Fifty percent of cervical cancers are caused by type 16, and another 20% are caused by type 18, but there are several other high-risk HPV types that can also cause cervical cancer,” Dr. Levinson said. “The vaccine won’t cure one if you already have it, but it will prevent you from getting any of the types you have not previously been exposed to.”
The development and approval of self-administered tests is progress and provides an opportunity to expand accessibility and improve early detection. Understand your personal risk and develop a relationship with a provider engaged in your care to ensure you receive the best recommendation possible for you and your health.